For centuries, the mind and the stomach have been linked in folklore - "gut feelings," "butterflies in the stomach," and stress-induced ulcers. Now, science is catching up with intuition. The gut and brain are connected by a sophisticated two-way communication system known as the gut - brain axis, and researchers are beginning to harness this pathway to reshape mental health itself.
A new review in the Mediterranean Journal of Medicine and Medical Sciences explores the promise of psychobiotics - live microbes that, when ingested in the right amounts, can positively influence mood, cognition, and even psychiatric disorders. Once considered fringe, the idea that bacteria could alter the mind is now gaining traction across neuroscience and psychiatry.
How microbes talk to the mind
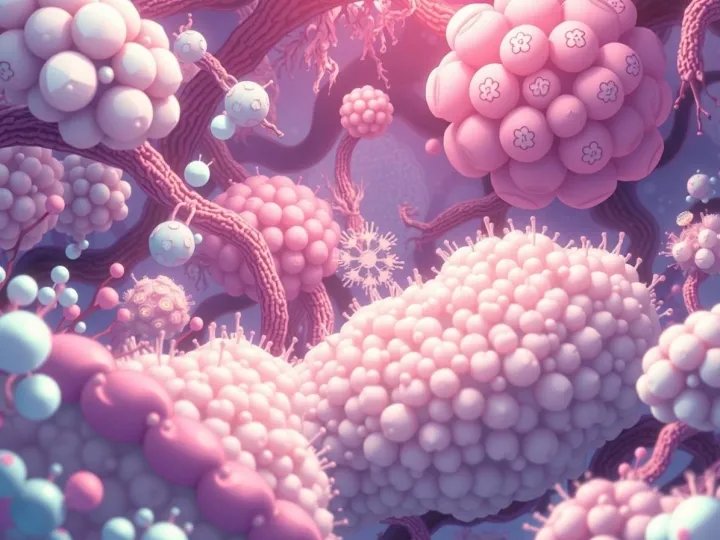
The gut - brain axis functions as a dynamic feedback loop. Signals travel along the vagus nerve, through immune pathways, and via a chemical alphabet of neurotransmitters. Microbes in the gut are active players in this dialogue. Certain bacteria can produce serotonin, dopamine, or GABA - the same molecules targeted by antidepressants and anti-anxiety drugs. Others regulate the body's stress response through the hypothalamic - pituitary - adrenal (HPA) axis, or protect the intestinal lining so inflammatory molecules don't leak into circulation and affect the brain.
This microbial influence helps explain why psychiatric disorders often overlap with digestive issues. Depression and irritable bowel syndrome, for example, frequently co-occur. By rebalancing the gut ecosystem, psychobiotics may ease both sets of symptoms at once.
The new frontier: engineered microbes
What makes today's psychobiotics different from the probiotics on supermarket shelves is engineering. Researchers are moving beyond off-the-shelf yogurt strains to develop precision microbes tailored to specific mental health outcomes. Techniques include genetic editing to boost production of key neurotransmitters, nanotechnology for targeted delivery, and even AI-driven personalization based on an individual's microbiome profile.
Early studies suggest such innovations could improve resilience to stress, reduce neuroinflammation linked to Alzheimer's disease, or support neurodevelopment in conditions like autism spectrum disorder.
Promise and caution
Despite the excitement, challenges remain. Microbial therapies must prove they can be delivered safely and consistently across diverse individuals. Regulatory bodies are still grappling with how to classify engineered psychobiotics - are they drugs, foods, or something entirely new? And ethical debates loom over how far society should go in redesigning the microbiome to alter mental states.
The review emphasizes that large-scale, long-term clinical trials are essential. Without them, psychobiotics risk becoming another overhyped wellness fad rather than a validated medical breakthrough.
A new chapter for psychiatry?
If the promise holds, psychobiotics could transform how we treat mental illness. Instead of simply blocking symptoms with pharmaceuticals, clinicians could guide the gut ecosystem itself, enlisting bacteria as allies in restoring balance to the brain.
For now, the gut - brain axis is reminding us of an ancient truth with modern science: the mind does not live in isolation. It is part of a complex biological network - one that begins in the gut and may hold the key to the future of mental health.